
October is National Breast Cancer Awareness Month: Do your part to knock out the disease
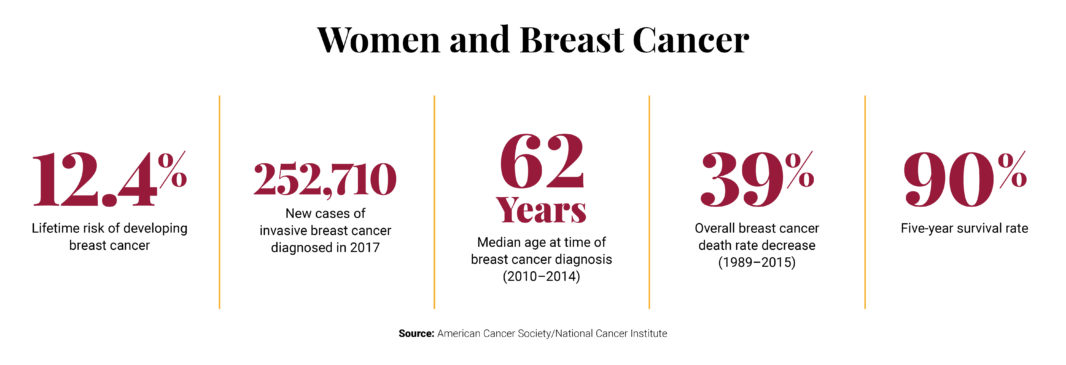
A woman living in the U.S. has a 12.4 percent risk of being diagnosed with breast cancer in her lifetime, and that risk only increases with age, according to American Cancer Society data.
Many women today know at least one person close to them who has been affected by breast cancer, and with early detection being paramount for survival, the more you know, the more likely you are to beat it.
What Is Breast Cancer?
Breast cancer is a disease in which cells grow out of control and can metastasize, or spread, to other parts of the body. Most breast cancers begin either in the breast tissue made up of glands that produce milk, called lobules, or in the ducts that connect the lobules to the nipple.
How Can I Detect Breast Cancer Early On?
There aren’t many distinct symptoms of breast cancer, besides the most common one: a painless lump felt in the breast. However, sometimes breast cancer spreads to the underarm lymph nodes and causes swelling, even before the original breast tumor grows large enough to be noticed.
According to Robin Reed, M.D., assistant professor at Tufts University School of Medicine, less common symptoms of breast cancer include blood or milky nipple discharge, or the skin around the breast has an “orange-peel” or “dimpled” appearance.
“We all know someone who has had breast cancer, but most have survived it,” says Reed. “It is not the death sentence it used to be, especially with early diagnosis.”
The general recommendation among physicians, including Reed, is that people should conduct a self-exam at home once a month, starting at age 18, as a way to become familiar with what their breasts usually feel like.
Although it is recommended, Reed says that breast self-exams, especially if done irregularly, can sometimes lead to over-diagnosing, fear, and unnecessary biopsies.
“Some women have more lumpy breasts than others. Get familiar with what’s normal for you.”
I Found a Lump; Now What?
It’s common for women, particularly those over the age of 30, to have breast lump concerns. Fortunately, most lumps are benign.
Reed says that many women have benign fibrosis cysts, which are what make up the texture of breasts. “Some women have more lumpy breasts than others. Get familiar with what’s normal for you, and if you notice a lump, see if it changes from before and after your period [if you are premenopausal],” she says.
Reed recommends to also check for swelling or lumps on the underarm lymph nodes, which may be another sign of breast cancer, at the same time that you check for breast lumps once a month.
“Our common sense goes out the window when we’re the one with a lump, so use your support system and medical providers to help you be more objective in evaluating any new lump,” says Reed.
When and How Often Should I Be Screening for Breast Cancer?

The Affordable Care Act covers mammograms at no cost every one to two years for women over 40
According to Reed, for the average woman, breast cancer is more common above the age of 50, which is why the U.S. Preventive Task Force recommends undergoing mammograms every two years for women ages 50–74. The Affordable Care Act covers screening mammograms at no cost every one to two years for women over 40.
The American Cancer Society and the American College of Obstetrics and Gynecologists have slightly differing recommendations. The ACS recommends women 40 to 44 years of age have the option to begin annual mammograms; women ages 45 to 54 years should undergo annual mammograms; and women 55 years of age or older may transition to biennial mammograms.
The ACOG recommends giving women ages 40 to 49 of average risk the option to screen annually and women ages 50 to 75 to screen for breast cancer either annually or biannually.
Reed says there is the downside of radiation exposure with mammography screening, so she recommends women ages 50 and up to screen every two years, unless “there is a specific lump being followed up on. In that case it is no longer called ‘screening’ but a diagnostic follow-up. Insurance will cover more frequent follow-up of discrete lumps than generic screening with no lumps.”
Digital or 3-D mammograms are a relatively new technological advance in screening, which more and more institutions are using now, says Reed. They result in more accurate imaging, but there is no difference in radiation exposure between regular and 3-D mammograms.
What Are the Factors Increasing the Risk of Breast Cancer?
Compared to women without a family history, risk of breast cancer is about two times higher for women with one affected first-degree female relative and 3-4 times higher for women with more than one first-degree relative, reports the ACA. A first-degree relative is a parent, sibling, or a child.
But those with a family history of breast cancer, fret not: The odds are still in your favor. The ACS also says that the majority of women with one or more affected first-degree relatives will never develop breast cancer.
According to the ACA, between the ages of 65 and 84, non-Hispanic white women have markedly higher breast cancer incidence rates than non-Hispanic black women. However, non-Hispanic black women have higher incidence rates before age 40 and are more likely to die from breast cancer at every age. Asian/Pacific Islander women have the lowest incidence and death rates for breast cancer.
Density refers to the amount of dense tissue (fibrous and glandular) compared to fatty tissue in the breasts. Women with dense breasts have more than double the risk of breast cancer.
Other risk factors studied and considered in the medical community include age of first menstruation cycle; age during which women experience menopause; bone density; use of fertility drugs; use of hormonal birth control; and weight.
More encouraging news is that with improved treatment interventions, almost 90 percent of females survive five of more years after the diagnosis of breast cancer.
Local Breast Health Resources
165 Worcester St., Wellesley Hills
Less than a mile from the Waban T stop, free on-site parking
800-476-0577
450 Brookline Ave., Boston
Longwood T Stop, Brookline Ave @ Deaconess Rd stop on the 60 and 65 buses, Dana-Farber garage or valet parking available
617-632-3800



 5 min read
5 min read


